 Cervical Myelopathy
Cervical Myelopathy
**II-Imaging
***1 – Plain Radiography
Plain radiographs are still relevant despite the development of modern imaging techniques (Figures 1, 2, 3).


These should include the following views: Antero-posterior (AP), lateral, ¾ obliques and especially lateral dynamic films that cannot be easily obtained with CT and / or MRI.
Plain radiographs enable an overall assessment of the dimensions of the spinal canal and detect the existence of a constitutional canal stenosis-a predisposing factor for cervical myelopathy (49):![]() The antero-posterior diameter of the spinal canal measured from the middle of the posterior vertebral body to the nearest point of the spinous process is equal to or less than the antero-posterior diameter of the vertebral body: Pavlov index (64).
The antero-posterior diameter of the spinal canal measured from the middle of the posterior vertebral body to the nearest point of the spinous process is equal to or less than the antero-posterior diameter of the vertebral body: Pavlov index (64).![]() The presence of platyspondyly with widening of antero-posterior diameter of the vertebral body
The presence of platyspondyly with widening of antero-posterior diameter of the vertebral body![]() The articular processes are projected on the posterior part of the vertebral body.
The articular processes are projected on the posterior part of the vertebral body.
They show the characteristic lesions of cervical spondylosis predominantly at the C5/C6, C6/C7 and C4/C5 disc levels, and specify the number of levels involved. The following are shown:![]() Hypertrophy of the articular processes (facets)
Hypertrophy of the articular processes (facets)![]() Osteophytes (bone spurs) of the posterior joints, endplates and unco-vertebral joints
Osteophytes (bone spurs) of the posterior joints, endplates and unco-vertebral joints![]() Pinching of the intervertebral disc
Pinching of the intervertebral disc ![]() Ligamentous ossification.
Ligamentous ossification.
Disorders of shape of the spine (static deformities) are objectified: loss of physiological lordosis, inversion of curvature, degenerative spondylolisthesis and instability on dynamic films most often in flexion. Pathologies such a sequelae of cervical spine injury or predisposing factors such as congenital cervical fusion may be associated.
Of old, it was classical to measure the dimensions of the spinal canal on these images correcting for radiological magnifications but this has lost its relevance today as these measurements are performed on the CT scan.
***2-CT Scan
The CT scan is the reference examination to study the spinal canal; its accuracy in this disease is evaluated in some studies to be between 70 and 90% (23). Acquisition is done in contiguous fine cuts or continuous spiral cuts after intravenous injection of contrast medium. We consider horizontal cuts, sagittal and coronal reconstructed bone window images as well as "soft tissue” images. The dimensions of the spinal canal whose mean values have been established for years (14) are measured. (Table 3)
Canal stenosis or narrowing is considered when the antero-posterior diameter at the site of maximum lesions (C5/C6 or C6/C7) is less than 12 mm.
All radiological signs observed on standard radiographs are objectivated with more details on the CT Scan (Fig. 4, 5, 6):
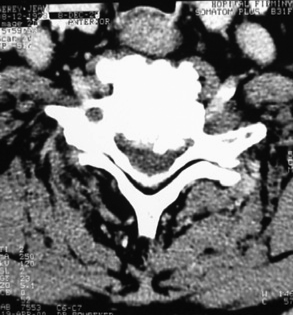
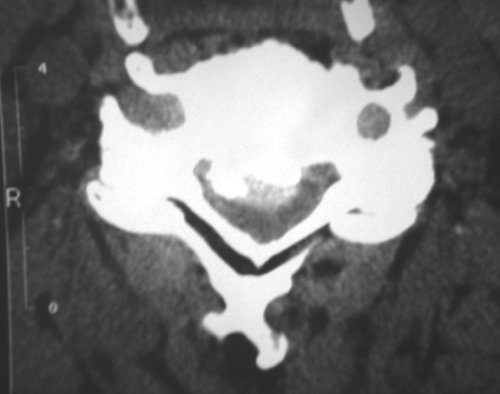

![]() On horizontal cuts: discopathies ("soft" or calcified), joint hypertrophy, facet joint osteoarthritis and ligamentous calcifications,
On horizontal cuts: discopathies ("soft" or calcified), joint hypertrophy, facet joint osteoarthritis and ligamentous calcifications,![]() On reconstructed images: the static spinal disorders (deformities) and degenerative spondylolisthesis.
On reconstructed images: the static spinal disorders (deformities) and degenerative spondylolisthesis.
CT enables a better appreciation of the components of the canal stenosis than conventional radiology:![]() Constitutional canal stenosis
Constitutional canal stenosis![]() Lesions related to the cervical spondylosis
Lesions related to the cervical spondylosis![]() "Soft" herniated disc
"Soft" herniated disc![]() Synovial cysts and associated pathology.
Synovial cysts and associated pathology.
The ossification of the posterior longitudinal ligament is easily demonstrated at the posterior vertebral body from which it is most often separate.
Dynamic films are difficult to do, but cuts can be achieved in extension or flexion by inserting pillows below the shoulders or under the head.
The CT Scan amongst others allows us to contrast between central cervical canal stenosis associated with a predominant central cord symptomatology (“sub lesional”) and lateral stenosis associated with a predominance of radicular semiology (“lesional”) in the upper limbs.
***3 - MRI
MRI is the paraclinical test of choice (2, 5). It enables the assessment of soft tissues and the repercussion of canal stenosis on the cord. Compared to intraoperative findings, the accuracy of MRI in the evaluation of lesions has been estimated at approximately 90% (10).
The MRI should include T1 and T2, sagittal, coronal and axial sequences. The injection of a paramagnetic substance (gadolinium) is usually not necessary (Figures 7, 8, 9, 10).
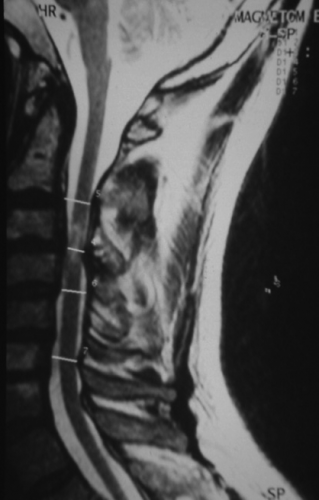


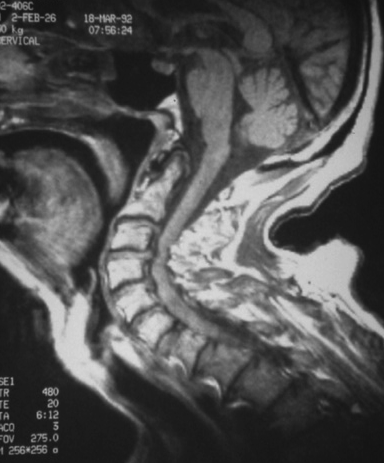
Like the CT scan, it is possible to carry out measurements of the spinal canal. MRI precises on the extent of stenosis contrasting segmental stenosis limited to one or two levels from extensive stenosis as well as the site of maximum anterior or posterior mechanical stress. It influences the decision as regards the choice of surgical technique. It may underestimate the ossified lesions.
Instability observed on plain films, can possibly be reproduced by performing sequences in positions where instability was observed.
The frequency of degenerative changes according to level varies thus: C2/C3: 25%, C3/C4: 14%, C4/C5: 25%, C5/C6: 56%, C6/C7: 44% (14).
T1 sequences give a better appreciation of the cord morphology that most often appears distorted and atrophic opposite disco-osteophytic projections or hypertrophied ligamentum flavum. The subarachnoid spaces appearing hypointense are difficult to analyze because can be confused for ligamentous structures which are also the same hypointensity. Disc and ligamentous calcification and osteophytes can cause an exaggeration of hypointense artefacts. The ossification of the posterior longitudinal ligament appears as hypointensity of varying thickness and widespread on the posterior surface of the vertebral body in front of the spinal cord.
T2 weighted images are the most useful sequences to study CSF which appears hyperintense. It is common to observe a thinning or effacement of the anterior or posterior subarachnoid spaces and a central cord hyperintensity at the site of maximum compression within adjacent segments. The significance of this hyperintensity is poorly understood. It is probably a cord edema related to repeated microtraumas. For some, it is not correlated with the severity of neurological lesion. With no prognostic significance, the cord signal may disappear after surgery (66).This is in contrast to what is observed in severe acute spinal cord injury where the hyperintense evolves either to a gliosis hypointense on T1 or syringomyelia. However, other studies are in favor of a relationship between the T2 signal abnormality and postoperative functional outcome (47). The hypointense on T1 in the spinal cord, which can also be observed in cervical myelopathy is usually not reversible after surgery and is associated with a poorer functional outcome (50).
In some cases, the central cord hyperintensity demonstrated by MRI has a characteristic "Snake-eye" appearance (two small areas of hyperintensity in the gray matter). This corresponds to a cystic necrosis secondary to mechanical compression and venous engorgement. The destruction of the gray matter in the anterior horn accounts for the resultant slower recovery of motor function in the upper limbs (56).
In the preoperative evaluation, information provided by the T2 sequences are sufficient to make the diagnosis and allows for non-consequential omission of T1 sequences (69).
***4 - Myelography and CT myelography
Myelography and CT myelography are indicated only when MRI is impossible to do or is contra-indicated. These studies can be complementary to the latter (75). They objectify the diameter of the spinal canal, anterior and posterior compressive elements whose topography can be median or paramedian (Figures 12, 13).


Compression may be severe to cause an interruption of the opaque column at the site of maximum stenosis.
Horizontal (axial) cuts enable the assessment of the dimensions of the cord which may appear atrophic and deformed: concave anterior surface, an anterior open “V-shape” deformation, and posterior displacement by bony spurs that may appear to be embedded in the spinal cord. Late films may opacify an intramedullary pseudosyringomyelic cavitation.
Myelography can realize dynamic images. The projections from discopathies are increased during flexion and those of the ligamentum flavum in extension. In case of instability it helps to objectify the aggravation of spondylolisthesis during flexion and its repercussion on the diameter of the spinal canal.
In some studies, the rate of accuracy of myelography in the diagnosis of cervical cord and root compression is greater than 80% (83).
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica

