Cervical Myelopathy
Cervical Myelopathy
**II-SURGICAL TREATMENT
The choice of the surgical technique is guided by the preoperative analysis of clinical and radiological findings, which in tend will determine the approach used. An anterior approach is performed in 85% of the cases by French-speaking European neurosurgeons; a posterior approach is performed in 15% of the cases while the use of a combined anterior-posterior approach is exceptional (12).
***1. Anterior Cervical Decompression (see: 71)
Described in the 1950s in the United States by Smith and Robinson (82) and in Europe by Dereymaker Mulier (22), this technique became popular from the 1970s through the work of Cloward (17) and Verbiest (90) to become a routine procedure in most cases. To the extended discectomies proposed by these authors have been added techniques median or anterolateral corpectomy.
The cervical spine is approached through an anterolateral route. The skin incision is horizontal (transverse) in a neck crease (Langer’s line) for a one or two level decompression and an oblique incision along the anterior border of the sterno- cleido-mastoid mucle for a more extensive decompression. After opening of the subcutaneous tissue and the platysma, the middle layer of the cervical fascia is incised along the anterior edge of the sterno- cleido-mastoid. The spine is approached in the space between the vascular sheath that is laterally retracted and the visceral sheath (pretracheal sheath) which is retracted medially. Usually, no vessels or muscles are sacrificed however it may sometimes be necessary to bind the superior thyroid artery and / or the omohyoid muscle. For right sided approaches to the lower cervical spine retraction should be moderate as not to cause injury by stretching the recurrent nerve whose course approximates the bisector of the angle formed by the inferior thyroid artery and tracheo-esophageal axis. For this reason, some authors prefer a left sided route where the left recurrent laryngeal nerve is deep and less exposed.
1.1. Discectomy with or without grafting (see: 71)
After radiological confirmation of the level, the anterior longitudinal ligament is incised using a scalpel and the disc is partially excised using curettes and fine rongeurs. At this stage, the operating microscope is introduced. After placing an interbody spreader, removal of the disc is done, leaving the cartilaginous end plates in place. If a sequestrated fragment has been expelled into the extradural space through a breach of the posterior longitudinal ligament, the latter may be partially resected to access the entire fragment expelled.
Resection of osteophytes is done if need arises with appropriate size rongeurs with the help of a diamond drill under visualization with the operating microscope and image intensifier. We can concomitantly perform via the same route an uncusectomy by removing the posterior 5 mm of the uncus. Resection is done from inside to outside with a 5 mm drill and with the aid of micro-curettes. Preservation of the anterior two thirds of the uncus prevents injury to the vertebral artery and postoperative instability.
At this stage of the procedure according to some authors, an intraoperative image guided injection of contrast material can be performed in situ (epidurography) to assess the quality of disco-osteophytic resection and achieve an immediate appropriate correction in case of insufficient decompression (35).
This type of “wide” discectomy can be done in stages, usually one to three. A complementary interbody graft can be used. The latter aims at preventing narrowing of the disc space that can lead to closure of intervertebral foramina as well as an eventual post-operative kyphosis. However, an analysis of the literature shows no significant difference between clinical series with or without grafting (27).
The "best" graft (ie, one that provides the best fusion rate) is the autologous tricortical iliac bone graft but the morbidity associated with graft harvesting (80) often leads to the use of allografts, xenografts or interbody cages filled with bone substitutes (Figure 16). Some authors are accustomed to performing a systematic complementary anterior osteosynthesis combined with interbody graft. This technique seems to provide a better restoration of disc height and lordosis at the operated level, and a higher fusion rate. Here again, comparative studies have failed to demonstrate significant clinical impact for patients treated with interbody graft plus osteosynthesis versus bone graft only (84). In case of instability, which can be observed in cases of very advanced degenerative disease, complementary anterior fixation may be associated with interbody graft.
The practice of French-speaking European neurosurgeons is extremely variable and depends more on habit, personal beliefs, school and tradition than on a significant difference in results (13): about 35% do not insert a graft, 26% bone graft without osteosynthesis, 17% place the graft in a cage to improve the mechanical properties and 15% combine a graft with osteosynthesis.
1.2. Cloward’s Technique (see: 17-18)
Once the discectomy and scraping off of the osteophytes is done, the width of the endplate is measured using a depth gauge. A strand of 12 to 18 mm in diameter selected according to the patient’s morphology most often 14 or 16 mm-is endowed with an abutment adjusted to the width of the endplate.This enables the drilling of a circular hole with a diameter corresponding to the straddling on the intervertebral space, starting from the adjacent endplates. The drilling of this hole enables the complete and safe removal of the posterior edges of the vertebral endplates seat of osteophytic proliferation. A trephine with a slightly greater diameter permits the trimming of the iliac graft whose outer diameter is equal to the inner diameter of the inter-vertebral hole, thus the graft perfectly fits into the drilled hole. However, and this being the main limitation of this technique, the thickness of the iliac crest, where the graft is taken, is often less than the width of the inter-vertebral space, thus the graft is often "short ".
1.3. Median Corpectomy (see: 73)
The approach is classic until the attainment of the anterior border of the concerned vertebral body (74).
Two techniques are possible: (i) if the discs are still present, the classical interbody approach should be done with resection discs at the end of the area to be decompressed (ii) if the ventral surface of the anterior column has been deformed by osteophytic degenerations which are sometimes asymmetrical, identification of the limits of the cervical furrow is more difficult. In the latter case, the inter-vertebral discs are generally completely collapsed making the trans-discal route impossible. We therefore first of all do a median trans-corporeal approach with a cutting drill, then with a diamond drill until we abut the posterior longitudinal ligament.
Corpectomy is initiated with the gouge forceps and then with a mechanical drill within a width of 10 mm until the posterior cortex is abutted and removed with 1 to 2 mm thick rongeurs. Upon contact with the dura mater, the corpectomy is widened to 12 or 14 mm. To obtain a satisfactory cord decompression, all the disco-osteophytic bars anterior to spinal cord that can cause injury should be resected. Bone resection should also include the endplates of adjacent vertebrae at the extremities of bone trough (gutter). Similarly, the posterior longitudinal ligament should be resected whenever possible but its adherence to the dura may make this procedure difficult.
At the end of the procedure, re-expansion of the dural sheath and the spinal cord appears as much as after a cervical laminectomy. The bone trough has the shape of a dovetail, broader at the rear- abutting the spinal cord-than infront. From either side, the lateral portion of the vertebral bodies-at the uncus is respected (preserved) to maintain spinal stability. The vertical extension of the corpectomy is tailored according to the preoperative radiologic findings, essentially MRI.
For most authors, the bony trough is filled with iliac crest or fibular autograft (possibly associated with osteosynthesis) which prevents the risk of postoperative kyphosis. Just as for discectomy, surgical practices are variable: 18% of Europeans neurosurgeons do not use grafts, 16% use an embedded bone graft without osteosynthesis and 66% use an embedded graft associated with osteosynthesis. Grafting does not seem necessary if precautions are taken to preserve the uncus (uncinate process) and if active rehabilitation of the muscles of the neck is done (88) (Figure 14).
***2. Posterior cervical ( cord) decompression
These are the oldest performed interventions. The patient is placed in the prone position, head slightly flexed, rarely in lateral decubitus position or sitting position. The lateral decubitus position allows for simultaneous anterior and posterior procedures. The skin incision is marked in the midline and the spine is reached at on the white line (ligamentum nuchae) separating the neck muscles retracted laterally.
2.1. Laminectomy (see: 17)
Laminectomy is the oldest technique performed. Initially, the spinous processes of the vertebrae are cut at their bases at their junction with the laminae. Bone resection brings out "en bloc" all the concerned spinous processes and the interspinous ligament. Laminectomy itself is performed by gradually removal of the laminae using fine bone rongeurs or even a mechanical drill. It is carried as far laterally as possible, even up to the inner part of the joints of which the lateral 2/3 should be preserved to avoid creating instability. The ligamentum flavum are usually fragmented along with the bone resection. This phase should be conducted with great caution given the narrowness of the spinal canal and the disappearance of the posterior epidural space caused by the pathology and worsened by the operative position.
Laminectomy may cause long-term kyphosis. The latter appears to be the result of insufficiency of neck muscles rather than bone and ligament instability induced by surgery (70). It can be prevented by appropriate early rehabilitation. Repeated progression of the disease is sometimes observed after laminectomy and has been attributed to the formation of a compressive epidural fibrosis (post-laminectomy membrane) whose pathogenic role however remains questionable (46).
2.2. Interventions preserving the posterior arch
To prevent postoperative kyphosis (86) and the formation of post-laminectomy membrane alternative technical solutions are possible.
2.2.1. The laminoplasty (see 39, 67)
Proposed as from 1970 by Japanese neurosurgeons, they are more difficult to carry out and do not appear more dangerous. Several technical variants have been described. (i) The "open door" technique is the most frequently performed. It consist of initially creating two paravertebral troughs at the junction of the lamina and facet while preserving the spinous processes and interspinous ligament, with the aid of a drill or a fine rongeurs at the side of the larger lesion over the entire length of the lower cervical spine from C3 to C7 at least to exceed all lesions, including, if necessary C2 and the first two thoracic vertebrae.
In principle, the ligamentum flavum is respected and the instrument does not penetrate into the vertebral canal, thus preventing root or spinal cord injury. On the other hand, on the contralateral side in the corresponding location only the outer cortical bone is drilled creating a trough to allow for “hinge-opening” of the lamina. The whole structure composed of the spinous processes, the interspinous ligament and the lamina is moved backwards by rotation (as if a door is opened "open door laminoplasty"). It is recommended to "open the door" for a distance at least equal to the diameter of the spinal canal, ie at least 12mm. The bony block moved backwards is fixed away from the dura matter by attaching it to the paraspinal muscles or better still by interposition of a spacer (spacer), consisting mainly of hydroxyapatite bone substitute, autograft taken from the spinous processes, in bioabsorbable materials of lactic acid polymer filled with cancellous bone or allograft. If the yellow ligament is not adherent to the laminae and stays in place, it should be resected secondarily (91).
(ii) The "double door" technique consists of opening the cervical canal in the midline. By the means of a high speed mechanical drill the spinous processes and the laminae are divided in the mid line to their point of contact with the ligamentum flavum, and the thinning of the lamina to their insertion at the facet joints. The opening of the vertebral canal is performed by introducing a spacer between each half of the spinous process, as in opening the portal of a double door. It is recommended to introduce spacers of bone substitute between the two halves of the spinous to keep them apart.
2.2.2. Laminectomy with preservation the spinous processes
Described by C. Large (31) in the lumbar spine, it is a unilateral para-vertebral route where the spinous processes are cut at their base via a trough at the junction between the spinous process and the lamina. The tissue bulk consisting of the spinous processes and the interspinous ligament is retracted beyond the midline exposing the laminae. Laminectomy is then conducted in a conventional manner. During closure of muscles, the interspinous ligament and spinous process fit back into their natural position on the midline.
2.2.3. Skip laminectomy ("Alternate" Laminectomy) (see 79, 81)
It concerns only alternate laminae: for example to achieve decompression from C3 to C7, only the laminae of C4 and C6 are resected and decompression is performed by resection of the ventral surface of adjacent laminae left in place. In addition, the interspinous ligament is preserved: the laminae to be resected are targeted by sectioning of the spinous process in the midline using a high speed drill and each portion of the spinous process is retracted laterally to preserve the insertion of the supraspinatus muscle.
2.3. Posterior osteosynthesis
Due to the risk of kyphosis, some authors have proposed the routine performance of a complementary posterior osteosynthesis. This seems to be reserved for rare cases where surgical decompression requires resection of the facets and there is preoperative instability. The best technique is that of screw osteosynthesis of the facet associated with a posterolateral graft.
*** 3. Combined Interventions (see 44)
In case of severe stenosis, a double approach simultaneously or in two successive staged operations can be performed. In this case, the risk of postoperative instability is relatively high, and decompressive surgery must be accompanied by grafting and anterior osteosynthesis with screwed plates into vertebral bodies.
***4 -Lateral spinal decompression
Described by George (15), this approach may become an alternative to standards anterior approaches.According to its author, this lateral approach could be indicated where anterior compression is predominant and the spine is straight or kyphotic without instability and without bilateral radiculopathy.
With this approach, after a direct control of the vertebral artery, the lateral portion of the intervertebral discs, vertebral bodies, the posterior longitudinal ligament and ipsilateral unco-vertebral joint can be resected if necessary depending on the extent of the lesions.
The advantages of this technique are wide exposure, the lack of need for graft and / or osteosynthesis, no contra-indication in case of kyphosis without instability and the the possibility of reoperation after a prior standard anterior cervical approach.
***5 - Indications
Early and simple forms in the elderly (JOA Score> 12) may justify trial of medical treatment with regular clinical follow-up (54).
Surgical treatment should not be delayed in young patients and when faced with any progressive form. It has been shown that the length of symptoms has more influences on the outcome than age, severity of illness, number of levels operated and/or pre-operative functional score (40).
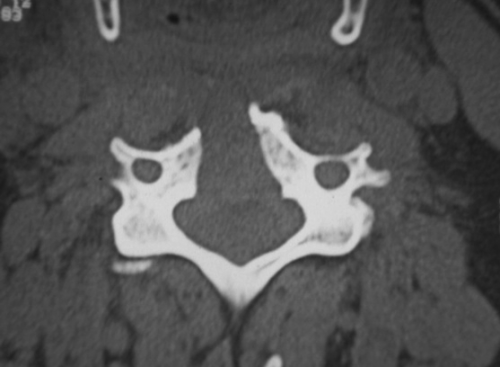
Imaging allows for the assessment of the lesions:![]() Anteroposterior and transverse diameter of the spinal canal,
Anteroposterior and transverse diameter of the spinal canal,![]() Overall appearance or segmental nature of the stenosis,
Overall appearance or segmental nature of the stenosis,![]() Number of levels affected
Number of levels affected![]() Predominant site of the compression: anterior or posterior
Predominant site of the compression: anterior or posterior ![]() Medial or lateral compression,
Medial or lateral compression,![]() Potential instability associated with stenosis assessed on dynamic films taken with caution
Potential instability associated with stenosis assessed on dynamic films taken with caution![]() State of the spinal cord: atrophic, intramedullary hyperintensity (cord signal).
State of the spinal cord: atrophic, intramedullary hyperintensity (cord signal).
Evoked potentials (somatosensory and motor) (48, 60, 68) could possibly help in the choice of surgical approach in case of difficulty in identifying the responsible clinical and radiological elements causing the compression: anterior or posterior.
The approach, anterior, posterior or combined, the extent of decompression and the indication for additional osteosynthesis will be chosen based on the results of these tests (93) bearing in mind that the anterior approach is preferred in terms of its simplicity and efficiency.
5-1 Indications of anterior approaches
The best indications for the anterior approach when there is myelopathy or myeloradiculopathy are represented by: (i) the presence of clinical signs predominantly in the upper limbs, from root lesion (myelo-radiculopathy) or central cord syndrome (brachial diparesis); (ii) the predominance of anterior compression elements (discs, osteophytes) over posterior factors (laminae, ligaments, facets), (iii) the existence of a preoperative cervical kyphosis.
5-1-1 Indications of discectomy:
Simple discectomy at one, two or three levels can be used if the lesions are limited to the disc levels responsible for segmental stenosis with the compressive elements close to the midline. Similarly, the anterior approach can be used as a complement to a posterior route if there is a persistence of anterior compression or as treatment for an evolving post-laminectomy kyphosis. The use of complementary interbody graft is more a matter linked to the schools of thought than the quality of long-term clinico-radiologic results (27). In general, the graft diminishes the severity of post-operative neck pain and frequency of late kyphosis, without being able to remove them completely. Complementary osteosynthesis is only exceptionally indicated in patients with preoperative instability; correctly performed isolated discectomy does not destabilize the spine.
5-1-2 Indications for median corpectomy
In affections involving three levels and / or in case of associated global stenosis a corpectomy can be discussed instead of the preferred laminectomy by some because in 75% of the cases the compression factors are anterior.
Additional graft is not necessary if the bony trough respects the uncinate processes (88). Reconstruction with bone graft and an eventual osteosynthesis is necessary when instability is certain (resection of one of the lateral columns) or when there is a tendency for instability, especially when associated with laminectomy. The grafts are generally autograft from the iliac crest, and sometimes from the tibia, allografts from graft bank, rarely xenograft or bone substitutes. Rare cases of instability with formation of kyphosis have been observed after simple corpectomy without grafting. It is therefore necessary to respect a rigorous technique and no hesitation to perform complementary grafting if in doubt of future stability.
5-2 Indications for posterior approaches
These approaches are preferred to anterior approaches when: (i) Clinically, patients show isolated or predominant signs of myelopathy, with a preponderance of posterior column affection over pyramidal signs (ii) anatomically, patients have extensive constitutional stenosis (rare situation) and / or predominantly posterior lesions: hypertrophic laminae, yellow ligament hypertrophy, hypertrophy of the facets.
"Standard" laminectomy is the easiest procedure to perform. The laminoplasty is preferred by Japanese and North American authors. The procedure is longer, more difficult and its superiority in terms of performance compared to standard laminectomy has not been demonstrated (57). Osteosynthesis is only associated in case of obvious preoperatively instability.
5-3 Indications for combined approaches
In our experience, the indications of mixed(combined) approaches are rare and are limited to severe stenosis with equivalent anterior and posterior lesions. They are sometimes indicated with incomplete results from an initial anterior or posterior decompression, or in case of recurrence of clinical signs after a period of improvement (44). A double approach can destabilize the cervical spine, thus the second operation should be accompanied by an additional fixation (44). If a double approach is done systematically, osteosynthesis with interbody graft should be done via an anterior approach: this is where it has the best biomechanical properties.
***6 - Results of treatment
Langston t. HoLLy, M.D.,1 PauL g. Matz, M.D.,2 PauL a. anDerson, M.D., Clinical prognostic indicators of surgical outcome in cervical spondylotic myelopathy. J Neurosurg Spine 2009;11;112-118
In the English literature, the effectiveness of treatment is assessed by a modification (expressed in percentage) of the JOA score (more accurate than the Nurick classification) according to the following formula: (postoperative score - preoperative score) / (17 - preoperative score) × 100.
6-1 Results of medical treatment
Rigorously followed up medical treatment can stabilize the disease for several years when the affection is in its mild and slowly progressive form (95). Clinical follow-up of patients with mild forms (average JOA score = 14) and myelopathy from “soft disc” shows that 60% can be stabilized or improved on medical treatment consisting of: spinal immobilization and reduced physical activity. In contrast, about 40% will worsen and should be operated. The incriminated lesions may regress on MRI in approximately 50% of cases (51). The JOA score improvement may reach 80% in initially relatively benign forms.
6-2 The results of surgical treatment
Clinical improvement depends more on the quality of the decompression than on the choice of surgical approach when it is adapted to the type and topography of the lesions (93).
There are a few more complications related to surgery in patients over 70 years because of associated pathologies (34).
According to the JOA classification, clinical improvement for all techniques is on average 55% (range 20-80%).The quality of functional outcome deteriorates with time and is only more than 45% after 6 years of progression. This deterioration is related to the continued progression of degenerative lesions and spinal deformities, as well as the onset of associated diseases in older patients: for example; hip osteoarthritis, lumbar canal stenosis.
It is possible to identify many prognostic factors (41, 77, 94):![]() Age is not determining (94) when the general condition, the degree of disability and associated pathologies are taken into account: same degree of improvement was observed before and after 65 years but only in younger subjects can complete recovery be observed. The aim moreover is not the same; young patients want to resume their full activities while older patients just want to gain sufficient autonomy.
Age is not determining (94) when the general condition, the degree of disability and associated pathologies are taken into account: same degree of improvement was observed before and after 65 years but only in younger subjects can complete recovery be observed. The aim moreover is not the same; young patients want to resume their full activities while older patients just want to gain sufficient autonomy.![]() The duration of symptoms is one of the most important prognostic factors: better results are obtained if the duration of the disease is short, especially in patients over 65 years, which could correspond to symptoms of functional cord affection before the installation of irreversible anatomical lesions (43, 94).
The duration of symptoms is one of the most important prognostic factors: better results are obtained if the duration of the disease is short, especially in patients over 65 years, which could correspond to symptoms of functional cord affection before the installation of irreversible anatomical lesions (43, 94).![]() The severity of preoperative disability seems paradoxically a less important factor (94).
The severity of preoperative disability seems paradoxically a less important factor (94).![]() The antero-posterior diameter of the cervical spinal canal and the surface area at its narrowest portion seems a determining prognostic factors regardless of age (43).
The antero-posterior diameter of the cervical spinal canal and the surface area at its narrowest portion seems a determining prognostic factors regardless of age (43).![]() Intramedullary T2 hyperintensity (cord signal) on MRI may influence prognosis (47), but it is quite controversial and inconsistently reported in the literature (43, 77, 94).
Intramedullary T2 hyperintensity (cord signal) on MRI may influence prognosis (47), but it is quite controversial and inconsistently reported in the literature (43, 77, 94).![]() Preoperative instability observed mainly in older subjects does not seem to influence the prognosis (41).
Preoperative instability observed mainly in older subjects does not seem to influence the prognosis (41).
***7 - Complications of surgical treatment (see 8, 30)
Degenerative cervical spine surgery is currently well mastered by specialized surgeons (11).
General complications common to all surgical procedures are rare approximately 1%. This type of surgery should not be feared regardless of the patient’s age when functional disability justifies it. There are few contra-indications.
Specific complications related to the anterior approach can sometimes be observed, they are directly related to the surgeon’s experience. The most classical and most common is that recurrent laryngeal nerve palsy which may be observed in 0.2 to 16.7% of the cases (29, 87), especially in the vicinity of the lower cervical spine (C6/C7 and C7/T1) via right approach. It is prevented by minimizing the retraction of tracheo-oesophageal axis or systematically using the left side approach that is less easy for a right handed surgeon. It is usually reversible. Pharyngeal or esophageal trauma may be observed but are exceptional, estimated to occur between 0.02 and 1.49% (20). Injuries of the great vessels are rarely observed (8). The occurrence of a postoperative hematoma is documented in 1-11% of cases in some observations (29). This complication in the form of a neck mass, is responsible for dysphagia and puts the patient at risk of respiratory distress.
One can observe aggravation in the neurologic status regardless of the approach. A common complication of extended decompression (but not often reported in the literature and in hospitalization summary) is paresis of the fifth and / or sixth cervical root, observed in 1-15% of cases (28, 89). Its physiologic mechanism is unclear. It is possible that it occurs during the installation of the patient on the operating table from a lesion of the radicular artery, but also from the particular fragility of this root stretched when the cord moves after decompression (89). It is usually regressive. Aggravation of clinical manifestations occur in 0.2 to 5% of the cases depending on the series (28, 29). These are the consequences of a spinal cord injury that may occur during the installation of the patient (for example excessive head flexion during a posterior approach) or during completion of the bone resection which requires the introduction of fine instruments (curettes, rongeurs or mechanical drills ...) in a much narrowed spinal canal. Vascular phenomena can sometimes be the cause of this type of complication. The most dangerous procedure is probably the resection of bony and disc calcifications, on the anterior aspect of the dura mater which we must not try to remove at all cost, thus limiting the procedure to decompression.
The evolution of this type of complication is unpredictable and depends on the severity of the neurological syndrome found during recovery from anesthesia. Some may be permanently quadriplegia.
Mechanical complications related to the surgery are the most important to know as they compel the surgeon to adapt the technique to the patient’s semiology and spinal lesions:![]() Interbody grafts can be displaced in about 2% of the cases (29). This is often the result of a misconfiguration of autografts or inappropriate choice of bone substitutes. Some surgeons advise wearing a cervical collar for several weeks. It has not been shown that this reduces the frequency of the incident.
Interbody grafts can be displaced in about 2% of the cases (29). This is often the result of a misconfiguration of autografts or inappropriate choice of bone substitutes. Some surgeons advise wearing a cervical collar for several weeks. It has not been shown that this reduces the frequency of the incident.
Displacements of material for osteosynthesis used in complementing an anterior approach may be observed. This can cause destabilization of the spine and / or a wound of the posterior part of the esophagus. Although difficult to accurately estimate, the frequency of this complication is nevertheless exceptional, particularly because of the widespread use of systems including interlocking screws. In addition, the screw profile has been improved to the point that all “loosening” became very rare or occurs simply as a result of a technical foul.
![]() Pain occurring as a consequence of graft harvesting from the donor site are observed in 20% of the cases. This relatively high figure discourages many surgeons from using autografts in degenerative disease, although it is by far the best graft (80).
Pain occurring as a consequence of graft harvesting from the donor site are observed in 20% of the cases. This relatively high figure discourages many surgeons from using autografts in degenerative disease, although it is by far the best graft (80).![]() A post-operative kyphosis is frequently observed after an anterior approach as in the posterior route. The realization of a graft and / or osteosynthesis reduces this risk (84) but does not completely eliminate it while increasing the burden of the operative procedures. This kyphosis seems more related to the inadequacy of neck muscles (70) which should be subjected to postoperative physiotherapy according to the extent of the decompression. Prolonged wearing of a collar could lead atrophy of paraspinal muscles and increase the risk of kyphosis. Finally, the preservation of the uncinate process during anterior approaches and anterior half of the joints during posterior approaches decreases the frequency of these complications. It has been shown that interbody graft is not absolutely necessary after a median corpectomy (88), which thus reduces the risk of complications and the cost of the intervention. Laminoplasty for many authors (86), decreases the risk of kyphosis compared to laminectomy, but this was not shown in the meta-analysis conducted by Ratliff and Cooper in 2003 (67).
A post-operative kyphosis is frequently observed after an anterior approach as in the posterior route. The realization of a graft and / or osteosynthesis reduces this risk (84) but does not completely eliminate it while increasing the burden of the operative procedures. This kyphosis seems more related to the inadequacy of neck muscles (70) which should be subjected to postoperative physiotherapy according to the extent of the decompression. Prolonged wearing of a collar could lead atrophy of paraspinal muscles and increase the risk of kyphosis. Finally, the preservation of the uncinate process during anterior approaches and anterior half of the joints during posterior approaches decreases the frequency of these complications. It has been shown that interbody graft is not absolutely necessary after a median corpectomy (88), which thus reduces the risk of complications and the cost of the intervention. Laminoplasty for many authors (86), decreases the risk of kyphosis compared to laminectomy, but this was not shown in the meta-analysis conducted by Ratliff and Cooper in 2003 (67).![]() After a laminectomy, a fibrotic scar (post-laminectomy membrane) develops that could be at the origin of the late deterioration of postoperative outcome (67). This is one of the reasons that contributed to the development of laminoplasty. In fact, the pathogenic role of this fibrous scar is questionable (46).
After a laminectomy, a fibrotic scar (post-laminectomy membrane) develops that could be at the origin of the late deterioration of postoperative outcome (67). This is one of the reasons that contributed to the development of laminoplasty. In fact, the pathogenic role of this fibrous scar is questionable (46).![]() The fusion of one or more cervical segments leads to early degeneration of adjacent segments which could be the source of a new pathology in 3% of the patients each year and in 10 years, 15 to 20% of the patients could require further surgery (37). In our experience, this figure is much lower and it has been shown that if these lesions are frequent, they are often asymptomatic (45). There is no evidence till date (for lack of sufficient clinical experience) that the use of cervical disc prostheses reduces this risk significantly (9).
The fusion of one or more cervical segments leads to early degeneration of adjacent segments which could be the source of a new pathology in 3% of the patients each year and in 10 years, 15 to 20% of the patients could require further surgery (37). In our experience, this figure is much lower and it has been shown that if these lesions are frequent, they are often asymptomatic (45). There is no evidence till date (for lack of sufficient clinical experience) that the use of cervical disc prostheses reduces this risk significantly (9).![]() All cervical spine procedures (with or without fusion) lead to a restricted range of neck movement. This usually remains mildly debilitating and well compensated for by adjacent segments, especially as these is most often in elderly patients with decreased activity and diffuse degenerative lesions of the entire spine.
All cervical spine procedures (with or without fusion) lead to a restricted range of neck movement. This usually remains mildly debilitating and well compensated for by adjacent segments, especially as these is most often in elderly patients with decreased activity and diffuse degenerative lesions of the entire spine.
Despite the long list of potential complications each of which taken in isolation (beside donor site painful sequelae) is relatively unusual, surgical treatment should not be delayed in a patient with neurological signs related to cervical myelopathy.
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica