 PITUITARY ADENOMAS
PITUITARY ADENOMAS
4.3 Ophthalmologic Assessment
An Ophthalmological Assessment should be done once the adenoma exceeds the sella with suprasellar extension in contact with chiasm. Assessment should include visual acuity, computerized visual field, fundus (looking for optic disc palor or papillary atrophy which are of prognostic value). OCT (Optical Coherence Tomography) is important to detect alterations in the optic nerve and is of prognostic value 30,32. Lancaster’s test will be requested for depending on the clinic picture.
4.4 Imaging
Baseline Radiological assessment for pituitary adenomas
Nasal Anatomy (Figure 6 a, b, c) : Check for septal deviation, nasal spine, mega conchae or concha Bullosa (pneumatization of the middle turbinate) which must be carefully studied to predict the surgical approach by a CT of facial bones although an MRI may be sufficient. Pneumatization and septations of the sphenoid sinus should be studied. The absence of a sphenoid sinus (sinus Concha) is not a contraindication of the the trans-sphenoidal approach but requires experience as the surgeon will have to create a neo- sinus by drilling. Neuronavigation and intraoperative imaging are then particularly useful.
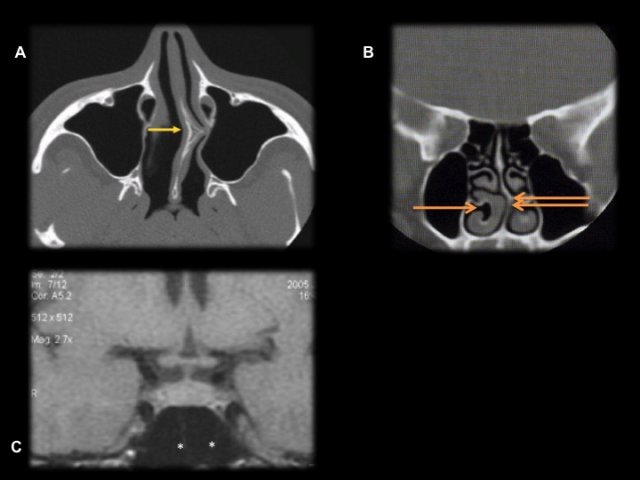
- Figure 6 : a : déviation du septum nasale avec épine ; b : méga-cornet inférieur ; c : la pneumatisation et les cloisons du sinus sphénoidal peuvent être étudiés sur l’IRM réalisée en pré opératoire.
MRI is the reference imaging for the pituitary and should have the following sequences: 2 to 3 mm coronal and sagittal slides for T1 weighted images with and without gadolinium-enhancement and T2 spin echo coronal sequences (Figure 7).
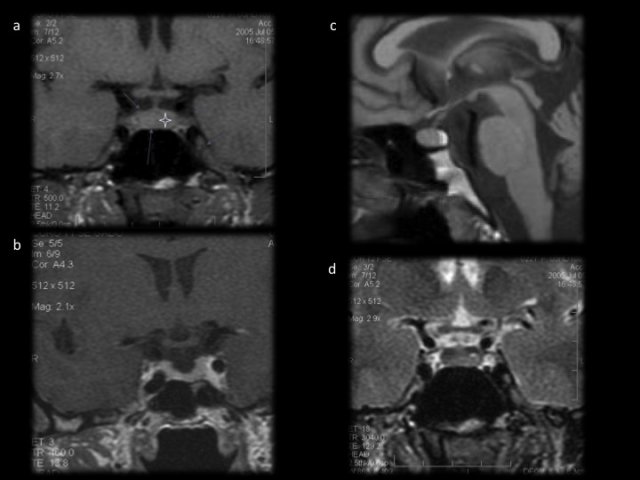
- Figure 7 : a : séquence T1 coronale sans gadolinium ; b : séquence T1 avec gadolinium, l’antéhypophyse se réhausse de façon homogène. c : en sagittal, la posthypophyse apparaît en hypersignal sur les séquences en T1 sans gadolinium. d : Image d’une hypophyse normale en T2 coronale. Les veines caverneuses sont parfaitement visibles.
A neuronavigation MRI (T1 gadolinium 3D sequences) is needed when planning for surgery. Special attention would be paid to detect cavernous sinus invasion. Two classifications (Knosp, Cottier) are in current use but invasion is still hard to say except in cases of encircled cavernous internal carotid artery (Figure 8).
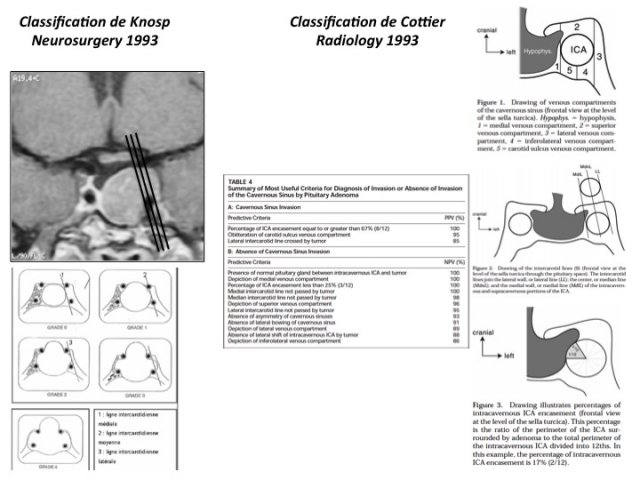
- Figure 8 : Classification de Knosp (à gauche) et de Cottier (à droite) concernant l’évaluation de l’envahissement des loges caverneuses.
The residual pituitary gland can often be seen even in cases of macroadenoma, as a hyperintensity at the upper part of the adenoma (Figure 9).
An evaluation of the tumor consistency is also of importance for the surgeon ; a firm tumor will be much more difficult to excise than a friable tumor. T2 W1 images are useful: a heterogeneous hyperintensity on T2 image is suggestive of a friable tumor while, a hypointense image would be in favor of a firm tumor. On Diffusion weighted images low signal would support a firm tumor 4 although this remains debatable 70.
Particularities according to type of adenoma
Somatotropic Adenoma
The densely granulated somatotropic adenomas respond more favorably to medical treatment. These adenomas may be detected by a low signal intensity on T2 W1 sequence. This however requires confirmation by complmentary tests 58.
In the absence of a pituitary adenoma on the MRI, a GH-RH assay with thoracoabdominal scan, and an Octreoscan be done to detect tumors responsible for ectopic secretion.
Corticotropic Adenoma
MRI sella is the routine test for the investigation of ACTH dependent syndromes (figure 5).
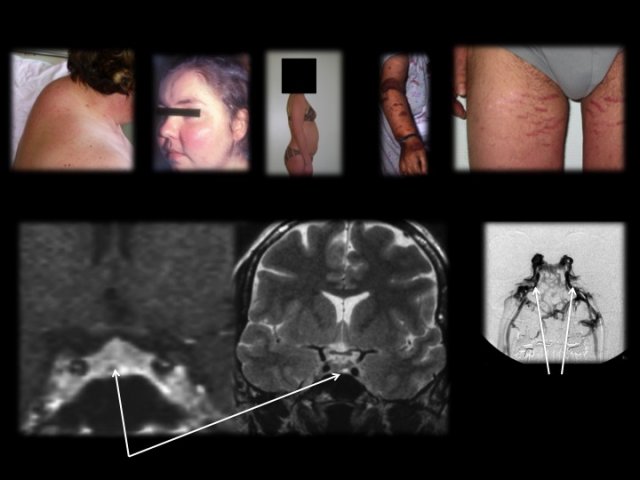
- Figure 5 : Photos du syndrome dysmorphique du Cushing. L’adénome est de type micro (flèche) parfois invisible sur l’IRM. En cas de négativité de l’IRM, un cathétérisme des sinus pétreux inférieurs est réalisé, le radiologue positionnant les micro-cathéters dans la partie verticale des sinus (flèches).
Dynamic images and possibly a 3D gradient echo T1-weighted sequence (ED3D) can be useful. The adenoma is often a microadenoma measuring few millimeters in the sella (intrapituitary) 55 and rarely macroadenomas (evolution of a silent corticotropic adenoma) 63. The absence of intrasellar mass should prompt for ectopic adenoma source (adenoma of the stalk, parasella, sphenoid or pharyngeal) 34,47.
In case of normal MRI, possibility of inferior petrosal sinus (IPS) catheterization should be discussed (Figure 5). The indication of IPS catherization should be well evaluated, because this involves patients with a fragile vascular field (risk of stroke). After IPS catherization, ACTH is assayed and the ratio of ACTH in IPS (closer to pituitary) or central value to the peripheral value is calculated. If this is spontaneously 2 or 3 after stimulation with CRH or desmopressin , this will be in favor of a pituitary origin 5,12. The value of the test in lateralization the assay to detect a right / left ACTH gradient is unreliable 79.
Atypical Adenoma and Carcinoma
MRI sella should be complemented by an extension work up if an atypical adenoma is suspected. A cranio-spinal MRI and a PET scan will be requested to search for secondary locations which will then ensure the diagnosis of a pituitary carcinoma.
Pituitary Apoplexy
No special investigations are needed. MRI imaging is the reference. CT Scan brain is however often done on an emergency basis to rule out subarachnoid hemorrhage. It will show a sellar tumor often hyperdense. MRI will show more or less infarcted tumor (hypointense on T1, hyperintense on T2) and haemorrhagic (T1 and T2 initially hyperintense).MRI enables the assessment of an extrasellaire extension and possible adenomatous residue (Figure 10). Thickening of the sphenoid sinus mucosa is frequently noted and sometimes correlated to the severity of the apoplexy 2,42.
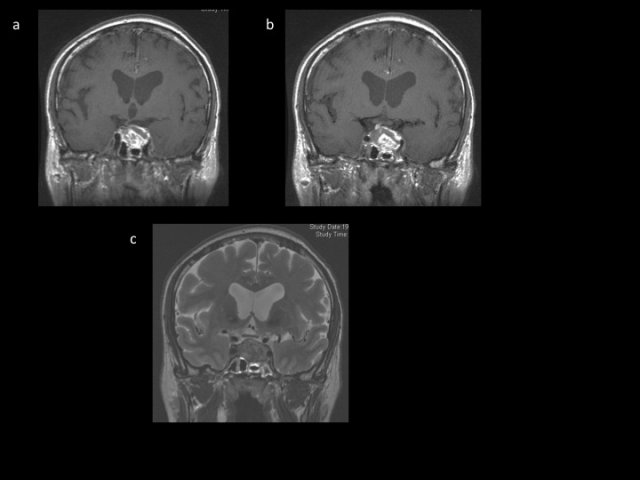
- Figure 10 : images d’apoplexie pituitaire phase aigue. a, séquence coronale T1 sans gadolinium : image en hyper et hyposignal hétérogène. b, séquence coronale T1 avec gadolinium : pas de rehaussement et pas d’image résiduelle d’adénome ou d’antéhypophyse. Extension vers la loge caverneuse gauche chez ce patient présentant une atteinte du III gauche mais pas à l’évidence d’envahissement latéral. A noter, l’image de « sinusite » sphénoïdale classiquement décrite dans les apoplexies pituitaires et corrélée à la sévérité du tableau d’apoplexie. c : séquence T2 coronale.
Differential Diagnosis
Sometimes a false diagnosis of pituitary adenoma is made on a patient a situation which one has to redress.
Other sellar or suprasellar tumors can mimic an adenoma. The most common are benign tumors such as meningiomas and craniopharyngiomas (Figure 11).
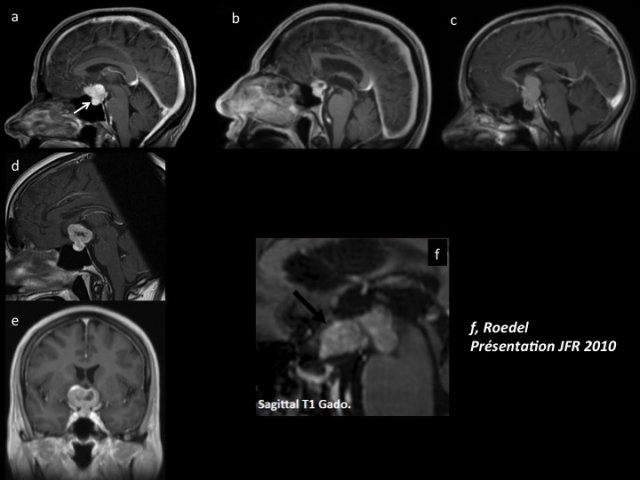
- Figures 11 : a : séquence IRM T1 avec gadolinium, sagittale montrant une image typique de méningiome (petite selle, insertion et développement sur le tubercule de la selle turcique, hypophyse visible au fond de la selle trucique) ; b : séquence IRM T1 avec gadolinium, sagittale montrant un craniopharyngiome (image hétérogène kystique et charnue) ; c : image de craniopharyngiome kystique ; d et e : séquence IRM T1 avec gadolinium, sagittale et coronale montrant une image à maximum suprasellaire dans un contexte de tumeur pulmonaire. Il s’agissait d’une métastase. ; f : séquence IRM T1 avec gadolinium, sagittale d’un lymphome. Tout comme le germinome, il s’agit souvent d’une image suprasellaire.
- Tuberculum sellae meningioma can mimic an adenoma. There are no specific clinical criteria. Radiologic discrepancy between a large suprasellar and a small sellar part is an important distinguishing feature. The dura tail sign with wide dura enhancement along the anterior and middle cranial fossae is also an important distinguishing feature. (Figure 11a).
- Craniopharyngioma: Less frequent diagnosis in adults (there is nevertheless a peak around the 5th decade). Anterior pituitary insifficiency is more common and posterior-hypopituitarism which is rare with pituitary adenomas may be present. Purely cystic sellar and suprasellar craniopharyngioma may be difficult to distinguish from a cystic adenoma (Figure 11c). The classic cystic-solid mixed form with some calcifications as well as suprasellar types are easy to distinguish an adenoma (Figure 11b).
- Other tumor types are rare. Metastases of sellar region are probably underestimated (Figures 11 d and e). The clinical setting (oncologic context, a posterior-pituitary insufficiency, oculomotor palsy) may increase the index of suspicion because the radiographic appearance is not specific. A malignant etiology should be suspected if osteolysis is present. The presentation may be variable between an enlargement of the pituitary stalk or sellar and suprasellar tumor. Lymphoma and germinoma involve particularly the infundibular and tuber region, show a strong contrast enhancement and often an anterior or posterior pituitary insufficiency clinically. (Figure 11f). Bipolar manifestations (pituitary and pineal) are characteristic of germ cell tumors.
- The distinction between cystic adenomas (Figure 12 a) and cysts of the sellar region can be problematic in routine practice (Figure 12).
- Rathke’s Pouch Cyst is hyperintense on T1 images in half of the cases (protein content), hyperintensity on T2 images with a non-enhancing intracystic nodule visible in T2 (Figures 12 d, e, f).
- The diagnosis of “Empty” Sella Turcica is made by the presence of dehiscence of diaphragma sellae with visualization of the pituitary on the floor of "balloned". sella. This can be accompanied by chronic hydrocephalus Figure 12 c).
- Sellar and Suprasellar Arachnoid Cyst (Figure 12 b) gives the same picture as the pituitary gland on the floor of the sella but with compressive mass in the suprasellar region. The patient is often middle or old age. Epidermoid or dermoid cysts, which are differential diagnoses of arachnoid cyst are often suprasellar but diffusion weighted images may help in the diagnosis
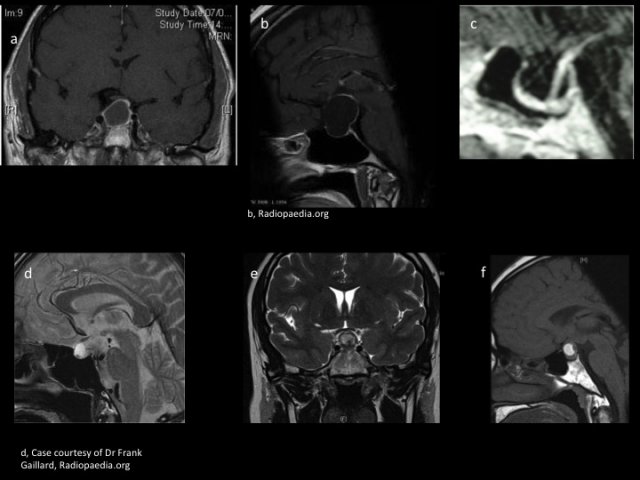
- Figures 12 : a : séquence IRM T1 avec gadolinium, coronale montrant un macroadénome kystique ; b : séquence IRM T1 avec gadolinium, sagittale montrant une image de kyste arachnoïdien ; c : séquence IRM T1 avec gadolinium, sagittale montrant une image de selle partiellement vide ; d, e, f : images de kystes de la poche de Rathke avec une image « de grelot » caractéristique en hyposignal T2.
- Inflammatory pseudotumors etiologies (neurohypophysitis, histiocytosis, sarcoidosis ...) are suprasellar with enlargement of the stalk and often with diabetes insipidus (questioning the possibility of the diagnosis of an adenoma) (Figures 13).
- The diagnosis of an inflammatory disease may be more difficult such as an adenohypophysitis of the pregnant woman (Fig. 13b). Occurrs in the last trimester or immediate postpartum and its image mimics that of an adenoma. It should be systematically thought of when the context is present.
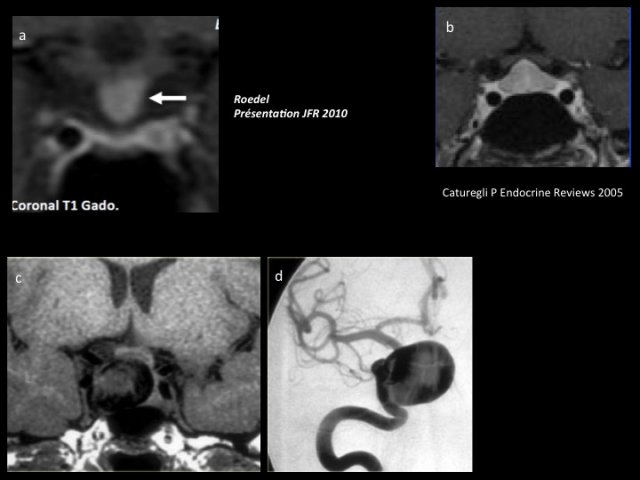
- Figures 13 : a : les atteintes inflammatoires type sarcoïdose (a) ou neurohypophysite atteignent souvent la tige et ne posent pas de problème diagnostic avec un adénome. L’adénohypophyse lymphocytaire de la femme enceinte ou du postpartum peut être plus difficile à différencier de l’adénome (b) ; c et d : l’anévrysme de la loge carotide étendu à la selle turcique se différencie aisément sous réserve d’y penser.
Pituitary abscess is rare ; is hypointense on T1 with peripheral enhancement in a clinical setting of fever and pituitary insufficiency.
Rare vascular etiologies must be kept in mind because of the consequences surgery. A dipping anterior communicating aneyrysm and the carotid-cavernous aneurysm distorting the sella can be misleading (Figure 13 c and d).
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica

