 PITUITARY ADENOMAS
PITUITARY ADENOMAS
1. Definition
Pituitary adenomas are tumors originating from cells of the anterior pituitary gland.
The pituitary gland or hypophysis (Figure 1) is an endocrine gland of approximately 10 mm in size consisting of two parts:
Anterior Pituitary Gland or Adenohypophysis which secrete the following hormones: ACTH (Adrenocorticotrophin Hormone), GH (Growth Hormone), TSH (Thyroid Stimuling Hormone), FSH (follicle Stimuling Hormone), LH (Lutropin Hormone), PRL (Prolactin) under the influence of the hypothalamus and
Posterior Pituitary Gland or Neurohypophysis secreting oxytocin (uterine action) and vasopressin or ADH (Anti Diuretic Hormone, antidiuretic activity) that controls urine output volume with respect to intake.
These tumors are usually benign and tumor cells retain some of the properties of pituitary cells secreting the aforementioned hormones.
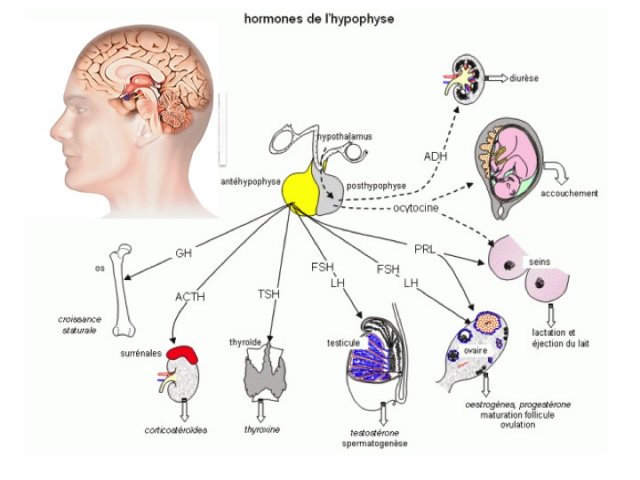
- L’hypophyse (figure 1)
2. History
The anatomy of the pituitary gland has been known since the Greek and Roman Antiquity particulary with the works of Hippocrates and Galen 29,43.
The latter made it to be believed that the pituitary was the route for the « disposal of waste products of the brain », a concept taught to medical students for millennia. The work of Vespasian 73 during the Renaissance raised questions about the concepts introduced by Galen but the relationship between « disease » and « pituitary tumors » only actually began with the introduction of anatomical and clinical methods in the 17th century.
Jean Louis Petit (1674-1750) showed that the development of a pituitary tumor can cause blindness 43.
Pierre Marie (1853-1940), in 1886, demonstrated the relationship between symptoms of acromegaly and pituitary tumor 46.
The link between Hypopituitarism and malfunction of the pituitary gland was established in 1901 by A Froelich (1871-1953) and H Cushing in his book "The Pituitary Body and Its Disorders" describing the different clinical pictures of hypo or hyper secretion 21,43.
3. Epidemiology and classification of pituitary adenomas
Pituitary adenomas represent between 10 and 20% of intracranial tumors in adults. They have a prevalence of 78 to 94/100 000 inhabitants and an incidence of 4/100 000 population with a tendency to increase with incidental findings ("incidentalomas")37. This is a rare tumor in children (2.7% of supratentorial tumors) 39 where the craniopharyngioma is the most common tumor in the sellar region.
With the advent of immunohistochemistry, several histological subtypes corresponding to different clinical pictures have been described.
There exist secreting or functioning adenomas: ![]() Prolactin secreting Adenoma or Prolactinoma (PRL) is the most common (60% of all adenomas, female-male ratio= 10/1, a prevalence of 440/100000 and an average age at diagnosis of 32 years)37.
Prolactin secreting Adenoma or Prolactinoma (PRL) is the most common (60% of all adenomas, female-male ratio= 10/1, a prevalence of 440/100000 and an average age at diagnosis of 32 years)37.![]() Somatotropic adenomas - Growth Hormone (GH) secreting adenomas represent approximately 13% of all adenomas with an estimated prevalence of 40 to 130 / million; age at diagnosis is 47 years37 with frequent variant-the somatoprolactininoma secreting both PRL and GH (50% of somatotropic adenomas).
Somatotropic adenomas - Growth Hormone (GH) secreting adenomas represent approximately 13% of all adenomas with an estimated prevalence of 40 to 130 / million; age at diagnosis is 47 years37 with frequent variant-the somatoprolactininoma secreting both PRL and GH (50% of somatotropic adenomas).![]() Corticotropic Adenomas have a prevalence of 0.17 / 10000037. These adenomas usally small (<10mm) or ’Micro-Adenomas " secreting ACTH and represent 6% of all adenomas. Macroadenomas are less common.
Corticotropic Adenomas have a prevalence of 0.17 / 10000037. These adenomas usally small (<10mm) or ’Micro-Adenomas " secreting ACTH and represent 6% of all adenomas. Macroadenomas are less common.![]() Thyroxin Adenoma secreting TSH is rare (<1% of all adenomas) with a prevalence of 0.15 / 2.8 million53. It is usually accompanied by hyperthyroidism, but it can be silent and multi-secreting (TSH-GH and TSH-PRL).
Thyroxin Adenoma secreting TSH is rare (<1% of all adenomas) with a prevalence of 0.15 / 2.8 million53. It is usually accompanied by hyperthyroidism, but it can be silent and multi-secreting (TSH-GH and TSH-PRL).
Apart from these secreting adenomas there exist non secreting or non-functioning adenomas (30% of pituitary adenomas). This term "non-functioning" is to be preferred because in about one third of cases 22,23,35, there is a hormonal expression, which can be used as biomarker although without clinical manifestations.
![]() These tumors are predominantly Gonadotropin Adenomas, from cells secreting FSH , LH or α subunit (these hormones ("gonadotropins") are glycoproteins composed of two subunits α and β).
These tumors are predominantly Gonadotropin Adenomas, from cells secreting FSH , LH or α subunit (these hormones ("gonadotropins") are glycoproteins composed of two subunits α and β).![]() Silent Adenomas are less common and usually considered as aggressive tumors. These are adenomas which present with manifestations of mass effects but without a specific clinical picture of hypersecretion. However in immunocytochemistry they are positive for ACTH, GH, or TSH or multiple hormones (GH or PRL and TSH and GH). Biologically, they either do not secrete hormones, or more frequently, they secrete an inactive pro-hormone explaining the absence of clinical signs or they produce hormones in small but measurable quantities (ACTH hypersecretion without hypercorticism is a frequent example).
Silent Adenomas are less common and usually considered as aggressive tumors. These are adenomas which present with manifestations of mass effects but without a specific clinical picture of hypersecretion. However in immunocytochemistry they are positive for ACTH, GH, or TSH or multiple hormones (GH or PRL and TSH and GH). Biologically, they either do not secrete hormones, or more frequently, they secrete an inactive pro-hormone explaining the absence of clinical signs or they produce hormones in small but measurable quantities (ACTH hypersecretion without hypercorticism is a frequent example).![]() Immuno-Negative Adenomas not reactive with antibodies are very rare (<5%). This is an undifferentiated form of gonadotropin adenomas.
Immuno-Negative Adenomas not reactive with antibodies are very rare (<5%). This is an undifferentiated form of gonadotropin adenomas.
Pituitary adenomas are considered as benign tumors but there exist aggressive or atypical adenomas and carcinomas. The frequency of occurrence of aggressive adenomas is still unknown; 15% grade 2b in the studies of Trouillas J et al. 75 and Laws80. Only 0.2% of tumors with metastases in their course are considered as carcinomas: mostly « secreting » - PRL-36%, ACTH-30%- and « non secreting » in only 23%. These metastases which are never inaugural occur 5-16 years after the onset of the clinical history and involve either the nervous system spreading via the cerebrospinal fluid (CSF) or are systemic : lung, bone, liver or lymph nodes (hematogenous spread ) 26. Patient survival is 4 years.
According to the WHO (World Health Organization) classification24, these tumors are classified into 3 types: Benign Adenomas, "Atypical" (strongly expressing p53, multiple mitoses, no threshold value for these two markers and a KI -67> 3%) and Carcinomas (with cerebrospinal or systemic metastases). This classification has no prognostic value because of no associated clinicopathological correlations.
The second classification which is more recent is a french multidisciplinary, multicentric case-control study of 410 patients with 8 years post-operative follow-up75.
In this study, invasion was defined by a radiological (MRI) and / or histological encroachment of the sphenoid sinus - with breaching of the dura and bone and especially the cavernous sinus 20,38.
Proliferation was defined histologically by the presence of two of the three following markers:
- Mitoses (n> 2/10 field at 40 magnification),
- A KI-67 index > 3% and
- A positive p53 (> 10 nuclei / 10 fields at 40 magnification).
Depending on the invasion and proliferation, 5 grades were defined (Figure 2): grade 1a: non-invasive, 1b: non-invasive and proliferative, 2a: invasive, 2b: invasive and proliferative, and 3: metastatic
This classification has proven to be able to predict remission and recurrence / progression at 8 years irrespective of the histological type. It individualizes the grade 2b tumors at high risk of residual tumor (25 times grade 1a tumors) or recurrences / progression (12 times grade 1a). The purpose of these classifications is to allow the clinician to rely on objective data to make complementry treatment decisions in cases of post-surgical residual.
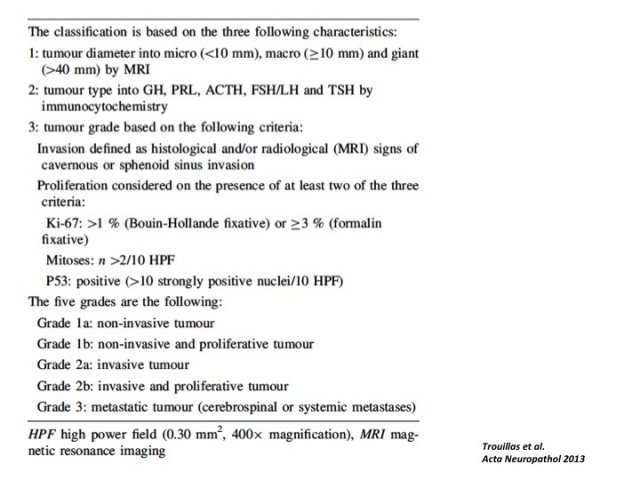
- Figure 2 : la classification des adénomes hypophysaires. Cinq grades ont été individualisés dans cette étude rétrospective multicentrique. Le grade 2b a été corrélé à des taux de récidive importants justifiant une vigilance accrue et une prise en charge plus agressive. Cela doit néanmoins être confirmé par des études prospectives.
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica

